The term “diastasis recti” (DR) often strikes fear and panic among those who have heard of it, or sheer confusion among those who haven’t (even trying to pronounce its name is difficult enough). And it’s no surprise. There is a great deal of mis-information and myths surrounding DR (a separation of the rectus abdominis muscle). We break everything down for you here in a clear and simple fashion — dispelling common myths, and setting the facts straight to hopefully give you some peace of mind and confidence on how to move forward.
What Diastasis Recti Is
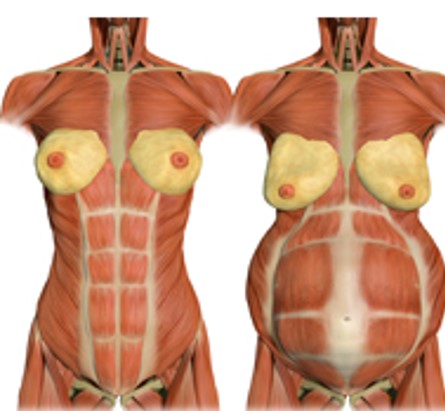
DR is a “wider than usual” separation of the left and right sides of the rectus abdominis (or “6 pack” muscle). One commonly used definition is a separation of 2.7 cm (about 2 finger-widths) or greater at the umbilicus (Rath et a., 1996). The word “diastasis” means separation, and “recti” refers to the rectus abdominis muscle. You can see a visual of how this might look below.

DR can often present as a “torpedo-like” protrusion in the belly. It is often easiest to see it during any movement that engages the abdominal muscles, such as in the images below.

Beyond the annoying “pooch-like” appearance, DR may indicate a weak and ineffective core. This can lead to a host of problems including low back pain, pelvic or hip pain, incontinence, constipation, or prolapse. It can also increases the risk of developing a hernia (when internal contents actually protrudes through a weak point in the abdominal cavity).
What Causes Diastasis Recti
The primary cause of DR is consistent and excessive intra-abdominal pressure (IAP). While it can happen to anyone — male and female alike — it is very common during pregnancy because a growing belly increases pressure in the core. Let’s explain further looking at the images below.
 The left side shows a non-pregnant individual. Here, you can see there is a tissue that runs down the midline of the body connecting the left and right sides of the rectus abdominis muscle. This tissue is called the linea alba. During pregnancy, consistent and excessive outward pressure from the growing belly stretches the linea alba (as you see in the image on the right), which thins and weakens it. When this happens, the left and right sides of the rectus muscle begin to pull apart, like you see in the image on the right.
The left side shows a non-pregnant individual. Here, you can see there is a tissue that runs down the midline of the body connecting the left and right sides of the rectus abdominis muscle. This tissue is called the linea alba. During pregnancy, consistent and excessive outward pressure from the growing belly stretches the linea alba (as you see in the image on the right), which thins and weakens it. When this happens, the left and right sides of the rectus muscle begin to pull apart, like you see in the image on the right.
It is important to note that some degree of DR is a normal and natural part of pregnancy. It is necessary to allow adequate space for the baby to grow, especially during the third trimester. In fact, some studies show that 100% of pregnant people experience diastasis recti during the 3rd trimester (Sptiznagle et. al., 2007). If managed well, DR can heal within the weeks or months following delivery.
Additional Factors that Contribute to DR
While pregnancy is one (normal and natural) cause of elevated IAP, there are other factors that can also increase the pressure in the core. The following activities further elevate IAP. So, when combined with a growing belly, they could exacerbate DR.
- Pregnancy Alignment Shifts: Neutral Alignment is key to reducing stress on your soft tissues. Unfortunately, the physical changes of pregnancy tend to pull your body out of neutral. You can see how the common anterior pelvic tilt (lower back arch) puts even more pressure on the linea alba tissue.

- Breath-holding upon exertion: This is also known as the Valsalva maneuver and is often used by weightlifters when lifting very heavy loads, as you see in the image on the left below. You may find yourself doing this when trying to lift a heavy object as well. Breath-holding upon exertion elevates the pressure in your core, which does lead to greater force production. However, it has the side effect of placing excessive pressure on your abdominal wall. This is also why DR can be experienced by powerlifters and athletes. Another example of breath-holding is bearing down on the toilet during a difficult bowel movement. While this can be an effective strategy if constipated, if used consistently over time, it can lead to issues with DR.

- Insufficient deep core strength: Your deep core muscles (diaphragm, transverse abdominis, and pelvic floor) help to regulate intra-abdominal pressure. If these muscles are weak, or fatigued, they cannot regulate pressure as well, which can lead to elevated pressure pushing outward onto the abdominal wall. For some beneficial exercises to strengthen the deep core, see the section on DR healing.
- Engaging in traditional core work in later stages of pregnancy, or too early postpartum: Pregnancy and early postpartum are periods in which the deep core is being taxed from the chronically-elevated IAP due to months of increasing weight gain and the stress from labor.
During the later stages of pregnancy (when there is an obvious belly), and in the initial postpartum stages (in which the core needs a gentle recovery focus), engaging in many traditional core exercises – such as sit-ups, weighted side bends, full planks, bicycles, V-sits, and leg lifts – could exacerbate DR because they further elevate IAP beyond that caused by the growing belly.
How to Spot DR
You may notice that torpedo-like protrusion in your belly during any movement that engages the abdominal muscles, as is shown in the images below. If you do notice this coning in any movement you do, simply stop that movement. That coning is a sign that the movement you are doing is not appropriate for your body at this time. It does not mean you will never be able to do the move again. It simply means that the current challenge exceeds the capacity of your core muscles.

Get the full Diastasis Recti Guide
For more detailed information on Diastasis Recti — including how to mitigate it during pregnancy, how to check for it in a manner that improves your testing accuracy, and strategies to kickstart healing — check out our complete Guide to Diastasis Recti below for just $27.
After completing your purchase, you will receive an email with a link to download your guide. If you have any questions, reach out to us at info@pronatalfitness.com.
BUY NOW
Sources:
Rath, A.M., Attali, P., Dumas, J.L., Goldlust, D., Zhang, J., Chevrel, J.P. (1996). The abdominal linea alba: an anatomo-radiologic and biomechanical study. Surgical and Radiology Anatomy. 18, 281-288.
Spitznagle, T. M., Leong, F. C., & Van Dillen, L. R. (2007). Prevalence of diastasis recti abdominis in a urogynecological patient population. International urogynecology journal, 18(3), 321-328.