While assessing postpartum clients for Diastasis Recti is standard practice, the check itself is anything but clear and simple. There are many variables that can influence the results, and even the most widely accepted definition of DR can be misleading when trying to get a true assessment of an individual’s core integrity or the degree of recovery work needed. This can certainly be frustrating for those looking to the DR check to provide precise measurements and clear guidance on how to proceed.
In this article, we’ll show you how to perform the assessment in a more accurate way to give you a clearer picture of the degree of recovery work needed. We will also discuss the variables that can influence your results so that you can improve your testing accuracy and more confidently proceed forward with recovery work.
When to Perform the DR Assessment
Recall that during pregnancy, virtually ALL people get DR by some point in the third trimester. Therefore, it is not really necessary to assess for DR during pregnancy because — especially in the later stages — because your client should have it. Moreover, many pregnant people are just not comfortable with you poking at their bellies. That said, if you see that a client is experiencing DR symptoms earlier in pregnancy, such as coning in the belly during movement, then you can perform this assessment provided your client is comfortable with it.
In the postpartum period, we recommend waiting at least 6 weeks to check for DR. This is because everyone has some degree of DR in the immediate aftermath of labor that may start to heal over the next few weeks on its own. So, waiting these 6 weeks will give you a little more accurate picture of the recovery work needed.
What to Check For
DR is a separation of the left and right sides of the rectus abdominis muscle (caused by an extreme stretching of the linea alba tissue that connects the two sides). Therefore, the first thing we are checking for is how far apart the left and right sides of the rectus abdominis muscle are. This is referred to as the inter-recti distance (IRD). While there is no standard definition of DR, the most well-accepted definition is an IRD (or gap) of 2.7 cm or greater (the equivalent of approximately 2 finger-widths or more). In other words, when you are checking to feel the distance between the left and right “ridges” of the rectus abdominis muscle, if you can fit two or more fingers in between those ridges, then this would be considered DR. Pretty simple right? Unfortunately, this definition that takes into account width only does not provide an accurate enough picture of the true severity of a client’s DR.
Newer research is revealing that depth of separation can actually be a more telling indicator of DR severity. In other words, when you press down on the gap, how “taut” (or not) does it feel? If the gap feels shallow, taut, and springy, this is a good sign. It indicates good integrity of the linea alba tissue. However, if the gap feels “soft and squishy” enabling you to sink your fingers down into the gap, this is a sign of a more compromised linea alba tissue, which will take longer to heal. Unlike the width measurement, there is no objective criteria for the depth measurement to assess severity. It’s really up to your own perception. The more testing you do, the better sense you will get for this.
When factoring in your width and depth assessments, the depth weighs more heavily on the speed of the healing process. As an example, a gap that is 3 fingers wide, but quite shallow, will likely take less time to heal than a gap that is 2 fingers wide, but deep.
How to Perform the DR Assessment
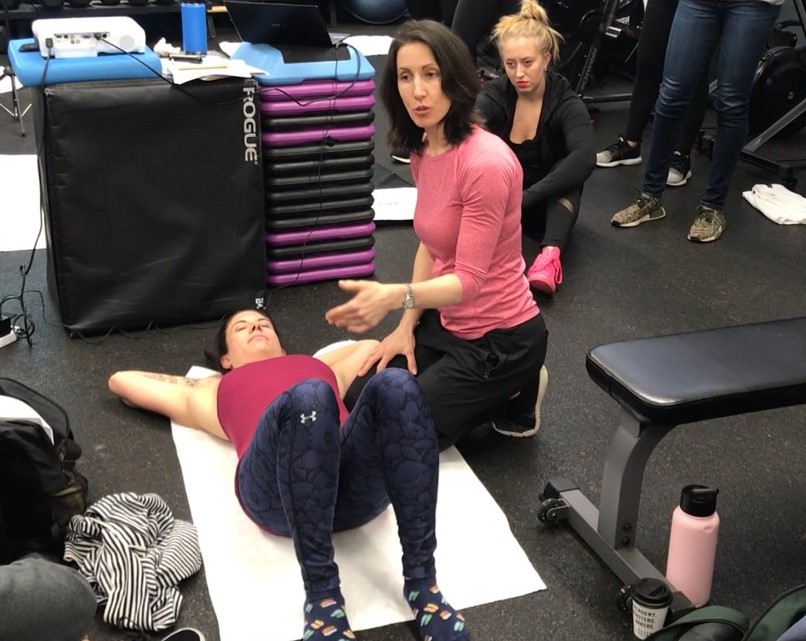
Watch the video below to get a basic overview of how to perform the client assessment. Then, review the recapped step-by-step process below. One important point to note. This video begins when the client is already on her back. When you perform the check, it is essential that your client transitions into the supine position safely by performing a Bed Roll. In other words, roll to the side first to get onto the back, then roll to the side when the assessment is complete in order to avoid any crunch-like movements.
Video Recap: Key Points to Remember
- Ask permission: Always ask your client permission to perform this check, as many people are not comfortable with their bellies being poked and prodded. If your client is not comfortable with you performing the assessment, teach your client how to perform a DR Self-Check
- Transition to supine safely: Have your client safely transition into the supine position by rolling to the side first. Then, place knees up with feet flat on the floor, and both hands behind the head.
- Perform the assessment at rest first: This can be tricky, especially if the client has excess abdominal fat. The purpose of doing this is to assess the difference in the tension of the gap from at-rest to with the head lift, so it’s good to have this baseline assessment of tension if possible.
- Ask your client to perform the head lift: After you’ve performed the at-rest check, ask your client to take a big inhale and, on the exhale, lift the head only about an inch off the ground. Begin to walk your fingers slowly down the midline – just as you did with the at-rest check – with your client continuing to exhale (allowing your client to rest as needed).
- Assess for width: With your client’s head lifted, begin to feel the separation by walking your fingers downward, noting the width of the medial borders (ridges) of the rectus as you progress down. Note how many fingers you can fit in between the left and right ridges (2, 3, 4, more?). Check all the way down until about 2 inches below the navel. Typically, the widest gap is at the navel, but not always.
- Assess for Depth: While you are feeling for gap width, also assess for depth. This is how the tissue feels when you press down on it. Is it shallow, taut, and springy (like there is some resistance when you press down)? Or is it soft, squishy, or deep (with little to no resistance when you press down)?
- Note comparison to at-rest check: When you assessed your client’s tissue tension (depth) with the head lift, did it feel different from the at-rest check? Did you notice that when your client performed the head lift, that you felt more tension or tightness in the gap? If so, this is a good sign. That means your client can generate tension in the linea alba. If you barely felt any difference at all, this is a sign of more compromised tissue.
- Roll to side to get up: Have your client safely return to a seated position.
Improving Your Testing Accuracy
While the DR test is an imperfect one that may yield slightly different results at different times, follow the tips below to improve your testing accuracy:
- Avoid test if client is feeling bloated: Don’t check if your client has eaten within the hour or is feeling bloated. Bloating pushes the abdominal contents forward, which widens the gap.
- Exhale when lifting the head (not after): Because we are trying to measure the best tension that the linea alba can generate, the way your client breathes during the assessment impacts the results. For the most accurate results, the client should exhale a split second before the head lift (completing the exhale with the lift). Avoid exhaling after the head is lifted.
- Lift no more than one inch: This is important. Many people will lift their heads up high like doing a crunch. This is especially common when performing a self-check as people want to see what they are doing. However, lifting the head too high will cause the gap to close a bit, which can make you think the gap is smaller than it really is. Lift only to the point where you feel the rectus muscles activate. This is typically about an inch off the ground.
- Apply consistent pressure: Note the pressure you apply when you test. Try to apply this same pressure each time you check because how hard you press down also impacts your results.
- When in doubt, assume DR: Sometimes it may be difficult to assess your client’s DR, especially in cases where there is excess abdominal fat following pregnancy. In these instances, you can simply assume DR. Core recovery work is beneficial at any point, so it’s always a good idea to take clients through this.
More DR Resources
To learn more about DR, and how to heal, see our resources below:
- Get the Guide to Diastasis Recti: This guide gives you more information about DR — including its causes (natural pregnancy causes and suboptimal behaviors) and some basic strategies to kickstart healing.
- Become a Pre/Postnatal Specialist: If you are a health and fitness professional interested in learning how to train pre & postnatal clients, explore our education to become ProNatal Certified. In this in-depth course, you will learn the ProNatal Core Recovery Protocol and how to utilize it on all types of clients to heal DR and build a truly strong and functional core.
Sources:
Lee, D., & Hodges, P. W. (2016). Behavior of the Linea Alba During a Curl-up Task in Diastasis Rectus Abdominis: An Observational Study. The Journal of orthopaedic and sports physical therapy, 46(7), 580–589.
Spitznagle, T. M., Leong, F. C., & Van Dillen, L. R. (2007). Prevalence of diastasis recti abdominis in a urogynecological patient population. International urogynecology journal, 18(3), 321-328.