A story from ProNatal Fitness Director of Education, Carolyn Appel.
I hand my 42 year-old client, Anna, the jump rope and tell her we are going to do three, 30-second skipping intervals. “OK, but let me go pee first,” she says.
I didn’t think twice about a client hitting the restroom before a bout of plyometrics because (1) it was relatively common and, (2) I remember having to do the same thing when I was a teenage athlete.
Over a dozen years later, I think back to Anna and the many other clients whom I failed. Not out of malice or neglect, but because I didn’t know any better. None of the continuing education conferences I dutifully attended ever mentioned Pelvic Floor Dysfunction (PFD), not even the pre and postnatal course I took as a green, new hire. So, I had no idea that Anna (or I) was experiencing a classic sign of PFD: accidental urine leakage during impact activities.
Does this story sound familiar to you? Unfortunately, PFD is too often viewed as an annoying, but normal, part of life. Perhaps this stems from the subject being too “taboo” to discuss in the past. Thankfully, discussions about the pelvic floor are becoming more mainstream today, so hopefully we are headed toward a shift in how we view this condition. Let us make one thing clear:
Just because it’s common, does not mean it’s NORMAL.
PFD is a core issue that — if not addressed — can lead to pain or other complications, and can certainly have a negative impact on one’s quality of life.
In this post, we’ll help you understand PFD, learn how to spot it, then importantly, provide you with some tips that can help you significantly improve your clients’ quality of life.
Your Pelvic Floor: Structure & Function
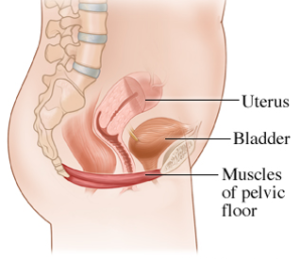
The pelvic floor (PF) is comprised of three layers of muscles (14 muscles in total), which form a sling at the bottom of your core. A well-functioning PF supports the pelvic organs, controls continence, stabilizes the pelvis, aids in sexual response, and assists in guiding a baby out during delivery.
Understanding Pelvic Floor Dysfunction
Now that we know what a PF is supposed to do, we can look at conditions that come from a poorly-functioning PF.
- Stress Incontinence: Accidental urine leakage during movements like coughing, laughing, sneezing, or any sort of impact activity in which there is a spike in intra-abdominal pressure. Fecal incontinence can occur as well, triggered by the same conditions as listed above.
- Pelvic Organ Prolapse: When one or more of the pelvic organs (bladder, rectum, or uterus) descends lower than its normal position, in some cases protruding through the vaginal or rectal openings. Often, it is described as a heavy, “bowling ball” feeling between the legs.
To help you determine if you might be experiencing PFD, review this Pelvic Health Self-Assessment from Pelvic Floor Occupational Therapist and PROnatal Advisory Board Member, Lindsey Vestal, of The Functional Pelvis. If you answer YES to some (or many) of these questions, you may be experiencing PFD.
What Causes Pelvic Floor Dysfunction?
Like Diastasis Recti, PFD is caused by a buildup of excess intra-abdominal pressure (IAP) that cannot be adequately managed. This is often a factor for pregnant people, whose growing belly and uterus place a great deal of excess pressure on the PF muscles (followed by the trauma of labor). However, there are many activities that add even more pressure beyond that caused by the growing belly. So, follow the tips below to mitigate this added pressure.
Keys to Mitigating (or Managing) PFD
- Coach neutral alignment: A growing belly during pregnancy tends to tip the pelvis forward into lumbar lordosis, as you see in the image below. The greater the anterior pelvic tilt, the greater the pressure on the PF muscles. Coach your clients into neutral alignment to help alleviate pressure on the pelvic floor.

- Teach 360˚ Breathing: One of the reasons we refer to 360˚ Breathing as the #1 most effective core exercise is because it gets the “Core Canister” to work together as a dynamic pump to regulate intra-abdominal pressure. Therefore, 360˚ Breathing helps regulate the pressure in the core (which is key to mitigating PFD).
- Avoid Breath-holding upon exertion: This technique, known as the Valsalva maneuver, is often used when lifting heavy loads. Holding your breath during the concentric phase of a movement spikes the pressure within the core. This results in greater force production. However, it has the side effect of placing excessive pressure onto the abdominal wall and pelvic floor. This is why PFD is relatively common with powerlifters or individuals doing heavy lifting. Another example of breath-holding upon exertion is “bearing down” on the toilet during a difficult bowel movement. While this can be an effective strategy if constipated, if used consistently over time, it can lead to issues with PFD.
- Avoid Sucking In & Chronic Engagement: While 360˚ Breathing helps to regulate pressure within the core, “sucking in” has the opposite effect. When you draw your navel in on the inhale, and hold tension there, it creates a pressure buildup in the abdominal cavity. Learn more about the negative implications of chronic core engagement to the pelvic floor (and other core muscles).
- Consider a Compression Garment: These can be effective in providing support, comfort, and leak protection. We love the medical compression garments from SRC health. They offer options for postpartum recovery and prolapse-specific garments. Use code PRONATAL10 for 10% off any purchase.
How to Begin Healing the Pelvic Floor
We always recommend seeking out a pelvic floor physical therapist as the best course of action when you suspect PFD. In addition, spend time practicing the pelvic floor exercises we refer to as PFAs (Pelvic Floor Activations). PFAs focus on:
- Activating all 4 pelvic floor attachment points: The pelvic floor muscles form a sling at the base of the core and have attachment points in the front (pubic symphysis), back (coccyx or “tailbone”), and sides (ischial tuberosities or “SITZ” bones).
- Working the muscles through a full range of motion (ROM): This means focusing on the eccentric portion of the movement just as much — if not more than — the concentric portion.
- Targeting slow and fast twitch muscle fibers: The slow-twitch fibers in the PF are responsible for supporting the pelvic organs and stabilizing the pelvic region. The fast-twitch fibers help to resist unwanted leakage (urinary or fecal). The two variations of PFAs that we teach (PFAs-Slow and Fast) target both.
Watch this video for a step-by-step process to first find your pelvic floor muscles and then learn how to perform PFAs-Slow and PFAs-Fast.
Many people also ask about “Kegels.” We do not use this terminology because Kegels have become synonymous with squeezing your pee-stopping muscles. However, as you know now, your “pee-stopping” muscles are only the front of your pelvic floor. Moreover, an over-focus on concentrically contracting (or “squeezing”) the muscles can lead to altered length-tension relationships and an overly tight pelvic floor, which can worsen PFD.
Additional Support
- If you have painful symptoms, consider wearing a compression garment. We love the range from SRC Health, which offers high-quality garments to wear under and over your bump (use code PRONATAL10 for 10% off).
- For programs and services to help you exercise safely and effectively during pregnancy, check out our training programs & services.
- If you are a health & fitness pro interested in coaching pre & postnatal clients, explore our ProNatal Education & Certification.
