It’s become so common, we’ve almost come to accept it as normal — that little bit of urine leakage when coughing, laughing, or doing any sort of impact exercise. We have somehow come to accept that “peeing your pants” a bit (or a lot) is just an annoying, yet normal, way of life.
But these symptoms are not normal. They are signs of pelvic floor dysfunction (PFD). PFD is a core issue that — if not addressed — can lead to other pains or complications, and certainly have a negative impact on your quality of life. Read on to learn more about PFD, it’s causes, and what you can do to kick start your healing.
Understanding Your Pelvic Floor
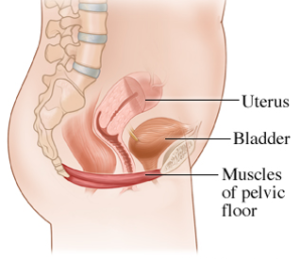
Your pelvic floor is comprised of three layers of muscles (14 muscles in total), which form a sling at the bottom of your core (or the “floor of the core”). Yes — your pelvic floor muscles are critical core muscles, even though they are often not the first to come to mind when we think of the core.
A well-functioning pelvic floor is responsible for:
- Supporting your pelvic organs: uterus, bladder, rectum
- Helping to stabilize your spine and pelvic-hip region
- Controlling continence (making sure you pee when you want to, and don’t pee when you don’t want to)
- Aiding in sexual response and satisfaction
- Assisting in guiding the baby out during delivery
Understanding Pelvic Floor Dysfunction (PFD)
There are basically two types of PFD:
- Stress Incontinence: Accidental urine (or fecal) leakage during forceful movements like coughing, laughing, sneezing, or impact exercise
- Pelvic Organ Prolapse: When one or more of the pelvic organs descends lower than its normal position (sometimes through the vaginal or rectal openings in the most extreme cases). It may feel like a heavy, bowling ball feeling between the legs. Pain during intercourse could also be a symptom.
For a more detailed list of symptoms, check out this Pelvic Health Self-Assessment by Pelvic Floor Occupational Therapist and founder of The Functional Pelvis, Lindsey Vestal. If you answer yes to many of these questions, you may benefit from speaking with a pelvic floor physical therapist.
Potential Causes of PFD
Like Diastasis Recti, PFD is in short a “pressure problem.” In other words, it occurs when there is a buildup of pressure in the abdominal cavity, and eventually that pressure has nowhere else to go, but downward onto the pelvic floor muscles. A growing belly and uterus during pregnancy certainly creates excess pressure, which is why PFD is so common during pregnancy.
Then, there is childbirth. Either delivery method — vaginal or cesarean — impacts the pelvic floor. In a vaginal birth, the pelvic floor muscles are responsible for helping to guide the baby out during delivery. However, if these muscles are underactive, or in a weakened and shortened state, this could result in increased tearing. A C-section also traumatizes the pelvic floor muscles because the procedure involves moving the abdominal muscles, which are intricately connected to the pelvic floor.
Tips for Mitigating PFD
Remember PFD is a “pressure problem.” While the physical changes of pregnancy add some pressure, it’s important to avoid activities that place further pressure on these muscles. Here are a few important tips to help alleviate undo stress on the muscles:
- Get in Neutral: Neutral Alignment is key to alleviating stress from your PF muscles. Unfortunately, the physical changes of pregnancy tend to pull your body out of neutral. You can see how the common anterior pelvic tilt (lower back arch) below puts even more pressure on the pelvic floor muscles. Learn how to find, and move in, neutral alignment.

- Master the #1 Most Effective Core Exercise: There are many reasons we refer to 360˚ Breathing as the #1 most effective core exercise. One of the many reasons is that it activates your deep “Core Canister” muscles to regulate the pressure in your core. The more of a 360˚ Breather you become, the less pressure you will place on your pelvic floor muscles. Learn 360˚ Breathing.
- Avoid “bearing down” or breath holding during exertion: This is a behavior we sometimes do automatically when lifting really heavy objects or pushing out a difficult bowel movement (envision “bearing down” on the toilet when constipated). Breath-holding upon exertion creates a spike in pressure within the core, which DOES create more power to lift or push, but also has the side effect of worsening PFD (and DR). This is why DR and PFD are actually common among powerlifters, or those who lift very heavy loads. Instead, focus on the principle discussed in the 360˚ article of exhaling on the effort and if you’re experiencing issues with constipation, follow these tips to help reduce constipation.
- Avoid “Sucking in”: Sucking your belly in, or holding it in a chronically taut position, is a behavior many people do for aesthetic reasons to make their bellies appear smaller. However, this action of drawing your navel in as you inhale, and holding tension there, creates a pressure buildup in the abdominal cavity. Learn more about the implications to your pelvic floor (and other core muscles) in this post on Why Sucking in Sucks.
- STOP constantly “engaging your core:” We often hear cues from instructors or trainers to “engage your core” or “draw your navel to your spine.” This action, when done on the EXHALE is beneficial during the strenuous portion of a movement. However, chronically engaging your core — or keeping your navel pulled into your spine — increases the pressure in your core. It’s like squeezing a tube of toothpaste. When you increase the pressure in the core, it has nowhere to go but downward onto your pelvic floor muscles.
Pelvic Floor Recovery Exercises
In addition to taking the steps above to reduce the excess pressure in your core, you can also practice some targeted pelvic floor exercises. We call this pelvic floor work PFAs (Pelvic Floor Activations). Watch the video below carefully to learn how to perform proper PFAs. We take you through a step-by-step process to first find all the muscles of your pelvic floor, then move them together in a coordinated fashion, and finally align the movement with your breath.
It is very important to note that if you are experiencing symptoms of PFD, the lengthening (relaxation) portion of PFAs is the most important. We recognize this may seem counterintuitive. After all, why would you want to relax those muscles when you have issues accidentally peeing?! Let’s make one thing clear:
A “tight” muscle is not a “strong” muscle.
On the contrary, a tight (or hypertonic) muscle is often a weak muscle. For example, imagine your bicep as the pelvic floor. When you perform bicep curls, you work through a full range of motion – lengthening your arm all the way down and curling it all the way up. Doing so is what helps to develop a strong, well-balanced muscle (or muscle complex) that can respond to various loads or impact.
Now, imagine you pick up a weight and just hold your arm in that flexed bicep curl position. After a while of the bicep being in this shortened (hypertonic) state, you would likely not be able to hold an object much heavier than your phone.
The same is true for your pelvic floor. If the muscles are held in a chronically shortened position, they will not be able to respond when needing to control larger amounts of force (like the force generated from sneezing, coughing, or jumping). That’s when “leaking” and other issues occur.
This is exactly why we avoid using the term “Kegel.” Kegels have become synonymous with “squeezing the muscles used to stop the flow of urine.” Hopefully by now, you see the two issues with this:
- Your “pee-stopping” muscles are only the front of your pelvic floor
- A focus on “squeezing” or contracting only can be problematic, especially for those experiencing symptoms of PFD
Additional Support
- If you have painful symptoms, consider wearing a compression garment. We love the range from SRC Health, which offers high-quality garments to wear under and over your bump (use code PRONATAL10 for 10% off).
- For programs and services to help you exercise safely and effectively during pregnancy, check out our training programs & services.
- If you are a health & fitness pro interested in coaching pre & postnatal clients, explore our ProNatal Education & Certification.
