Most of us are familiar with the idea (and the benefits) of undergoing physical therapy after a certain part of our body has experienced trauma (perhaps a major surgery, injury, etc.). However, we don’t often think about pelvic floor physical therapy to help the critical deep core muscles of our pelvic floor heal from the stresses of pregnancy and childbirth.
To help you understand what pelvic floor physical therapy is, and why it’s so important for everyone with vaginal anatomy — especially those who are pregnant or who’ve had children at any point — we turned to pelvic floor physical therapist, Ashley Rawlins, PT, DPT of Origin Physical Therapy, a leading provider of pelvic floor and whole-body physical therapy nationwide with a specialized focus on pregnancy, postpartum and sexual health.
Let’s begin with the basics.
What Exactly is the “Pelvic Floor”?
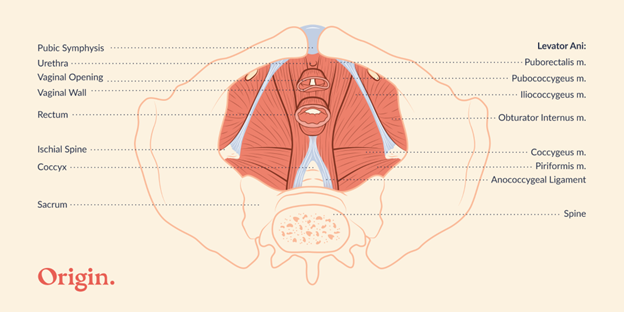
At the very bottom of your pelvis lies a bowl-shaped group of muscles and tissues that collectively make up what is known as your pelvic floor. It includes muscles that anchor at your pubic bone and tailbone, and wrap around the vaginal, urethral, and anal openings. The pelvic floor also includes the skin, nerves, and blood supply that help the muscles come alive.
What Role do the Pelvic Floor Muscles Play?
Your pelvic floor muscles are responsible for quite a few things, including coordinating with your diaphragm to help you breathe; contracting and relaxing to help you control your bowel, bladder, and sexual functions; and even working to provide stability and circulation throughout your pelvis. Like all of the muscles in your body, the pelvic floor muscles need to be strong, flexible, and coordinated in order to work effectively.
Most of these duties seem to happen automatically day in and day out, which is what can make the pelvic floor so mysterious. However, when the muscles become underused and weak, or overworked and tight, or they lose coordination from years of suboptimal habits, you may begin to notice symptoms of pelvic floor dysfunction.
What is Pelvic Floor Dysfunction?
Pelvic floor dysfunction (PFD) describes a group of symptoms that occur when the pelvic floor muscles aren’t working correctly. Very common life events such as pregnancy, childbirth, trauma, and menopause can all increase the chances of these muscles developing dysfunction. Symptoms commonly related to PFD include:
- Bowel or bladder leakage of any amount, including difficulties holding back gas, leaking urine or leaking stool
- Pelvic heaviness or a feeling that something is dropping in your vaginal or falling out
- Pain with sex, or other sexual dysfunction
- Pain anywhere in the pelvis or low back
- Difficulties with starting your urinary flow, or fully emptying your bladder
- Difficulties holding your bladder because of a sudden, strong urge to urinate
- Constipation, or feeling like you can’t fully empty your bowel
PFD is Common but not Normal
If you’re thinking many of the above symptoms seem quite common (especially among those who’ve had children), you are correct. In fact, here is what research shows us:
- Each year, 40 million women experience pelvic floor issues which are often easily prevented or treated with pelvic PT (Nygaard et al., 2008)
- 1 in 3 women have bladder leakage. This is notable within the first three months after having a baby, but also chances increase again as we age and move into menopause (Grodstein, 2003)
- 50% of women experience lower back pain during pregnancy. Having pain in pregnancy increases the chance of having long term pain in the postpartum (Katonis et al., 2011)
- Over 1 in 4 women have painful sex (Flynn et al., 2017). This is more common in the first year after having a baby with two-thirds of women reporting postpartum sexual dysfunction (Khajehei et al., 2015)
- Up to 70 % of women will experience changes in the bladder and sexual function, including increased bladder leakage, and sexual pain (Moral et al., 2018).
These numbers are just the tip of the iceberg when it comes to pelvic floor symptoms. Pelvic floor dysfunction is common, but let’s make one thing clear:
Just because it’s common, does not mean it’s NORMAL.
None of the above symptoms are normal. They are signs of dysregulation in the core, and can certainly impact one’s core strength and quality of life. The good news is when it comes to pelvic floor dysfunction, pelvic physical therapy is an evidence-based, highly effective treatment option for any of these symptoms (Wallace, Miller, & Mishra, 2019).
What is Pelvic Floor Physical Therapy?
Pelvic floor physical therapy (PT) is a specialized area of physical therapy that focuses on improving and restoring the pelvic floor. A pelvic floor PT will spend time getting all the details about your symptoms (there’s no such thing as TMI), working to fully understand your related health history, and examining your pelvic floor muscles. After conducting a thorough examination, and determining how your health history and muscle function interplay with your symptoms, your PT will collaborate with you to determine the most effective physical therapy program for you.
We understand that it can be intimidating to think about seeing a pelvic floor PT, especially if this is an area of your body that you find hard to discuss — or if you’ve brought your symptoms up to a healthcare provider in the past, only to have them dismissed or belittled. Seeing a pelvic floor PT will be a very different, and much more positive experience.
Book a FREE 10 Minute Consultation
If you think pelvic floor PT may benefit you, book a FREE 10 minute intro call with the experts at Origin Physical Therapy. Origin offers virtual and in-person PT sessions, covered by insurance and supported by proprietary exercise programs, educational content, and community experiences. Begin with this free introductory call to see how it might benefit you.
Post Contributor
Dr. Ashley Rawlins, PT, DPT is a doctor of physical therapy and Clinical Learning & Development Lead at Origin Physical Therapy. She has advanced certification in the treatment of Pelvic Health and Obstetric Health (CAPP-Pelvic, CAPP-OB). She specializes in the treatment of pelvic floor muscle dysfunctions including pelvic pain, sexual dysfunction, pregnancy related pain, postpartum recovery, and bowel and bladder dysfunction. She is a practicing clinician, educator, and author in the field of women’s health physiotherapy. She has taught courses on women’s health physical therapy to physical therapy students in Dallas, has provided education to groups throughout the community, as well as assisting in teaching continued education courses to physical therapists and other healthcare professionals. Her most important job is being a wife and mother to her silly, active little boy and sassy, precious daughter.
Sources
Flynn KE, Carter J, Lin L, Lindau ST, Jeffery DD, Reese JB, Schlosser BJ, Weinfurt KP. Assessment of vulvar discomfort with sexual activity among women in the United States. Am J Obstet Gynecol. 2017 Apr;216(4):391.e1-391.e8. doi: 10.1016/j.ajog.2016.12.006. Epub 2016 Dec 14. PMID: 27988269; PMCID: PMC5376372.
Grodstein F, Fretts R, Lifford K, Resnick N, Curhan G. Association of age, race, and obstetric history with urinary symptoms among women in the Nurses’ Health Study. Am J Obstet Gynecol. 2003 Aug;189(2):428-34. doi: 10.1067/s0002-9378(03)00361-2. PMID: 14520212.
Katonis P, Kampouroglou A, Aggelopoulos A, Kakavelakis K, Lykoudis S, Makrigiannakis A, Alpantaki K. Pregnancy-related low back pain. Hippokratia. 2011 Jul;15(3):205-10. PMID: 22435016; PMCID: PMC3306025.
Khajehei M, Doherty M, Tilley, P.J, Sauer, K. Prevalence and Risk Factors of Sexual Dysfunction in Postpartum Australian Women. The Journal of Sexual Medicine. 2015 Jun; Vol 12, Issue 6, P1415-1426
Moral E, Delgado JL, Carmona F, Caballero B, Guillán C, González PM, Suárez-Almarza J, Velasco-Ortega S, Nieto C; as the writing group of the GENISSE study. Genitourinary syndrome of menopause. Prevalence and quality of life in Spanish postmenopausal women. The GENISSE study. Climacteric. 2018 Apr;21(2):167-173. doi: 10.1080/13697137.2017.1421921. Epub 2018 Feb 7. PMID: 29411644.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ; Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008 Sep 17;300(11):1311-6. doi: 10.1001/jama.300.11.1311. PMID: 18799443; PMCID: PMC2918416.
Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019 Dec;31(6):485-493. doi: 10.1097/GCO.0000000000000584. PMID: 31609735.
